The Stark Law, or the Federal physician self-referral law, applies to nurse practitioners in certain contexts. For example, it applies when hospitals provide subsidies to physician practices for recruiting non-physician practitioners, including nurse practitioners. The Centers for Medicare and Medicaid Services (CMS) has created exceptions to the Stark Law, such as allowing hospitals, Federally Qualified Health Centers, and Rural Health Clinics to provide payments to physicians for recruiting NPPs like nurse practitioners to address healthcare provider shortages. Additionally, the Office of Inspector General (OIG) has issued advisory opinions approving arrangements where acute care hospitals employ nurse practitioners to perform certain services traditionally done by primary care physicians. While the OIG opinion addresses the Anti-Kickback Statute, similar arrangements may face obstacles under the Stark Law.
| Characteristics | Values |
|---|---|
| Stark Law | Federal physician self-referral law |
| Who does it apply to? | Physicians |
| Who does it not apply to? | Non-physician practitioners (NPPs) such as nurse practitioners, clinical nurse specialists, and certified nurse midwives |
| What is an NPP? | A clinical social worker, clinical psychologist, physician assistant, nurse practitioner, clinical nurse specialist, or certified nurse midwife |
| What is the purpose of the Stark Law? | To prevent abuses in the financial relationships between physicians and healthcare service entities with which they have a financial relationship |
| What is an example of a violation? | A hospital providing payments to physicians to assist in recruiting and employing NPPs |
| Are there any exceptions? | Yes, as of October 30, 2015, there are two new exceptions: recruitment support for physicians to hire NPPs, and physician timeshare lease arrangements with hospitals |
What You'll Learn
- Hospitals can provide subsidies to physicians for recruiting nurse practitioners
- Stark Law exceptions for non-physician practitioners
- Nurse practitioners can perform tasks traditionally done by physicians
- The Anti-Kickback Statute and its relation to nurse practitioners
- The impact of the Affordable Care Act on the demand for nurse practitioners

Hospitals can provide subsidies to physicians for recruiting nurse practitioners
The Stark Law, which relates to compensation arrangements involving the referral of certain designated health services, applies to nurse practitioners. A notable exception to the law permits hospitals to provide subsidies to private practice physicians to recruit and employ non-physician practitioners (NPPs) in high-need fields. This includes nurse practitioners, physician assistants, certified nurse midwives, clinical social workers, and psychologists.
The exception was created in response to significant changes in the healthcare system, including predicted shortages of primary care practitioners and an increased demand for NPPs. Hospitals can provide subsidies of up to 50% of NPP compensation, including salary, signing bonuses, and non-cash benefits. However, there are several conditions that must be met for this exception to apply.
Firstly, the arrangement must be unrelated to referrals and must be monitored and documented in detail. Secondly, NPP compensation must be at fair market value (FMV), which can vary by market, discipline, and specialty. It is the responsibility of the hospitals and physician groups involved to determine and document FMV. Thirdly, the NPP subsidy is only available once every three years to the same physician practice and can only be used to recruit an NPP who has been outside of the hospital's service area for at least one year.
While this exception can be a valuable tool for hospitals to attract new practitioners, it is important to carefully consider the potential challenges and costs associated with its use. Hospitals should establish their own NPP subsidy limitations and guidelines to ensure fair implementation and control costs.
In conclusion, while Stark Laws do apply to nurse practitioners, there is an exception that allows hospitals to provide subsidies to physicians for recruiting NPPs, including nurse practitioners, under specific conditions and within defined limits.
Retroactive Law: Past Actions and Legal Consequences
You may want to see also

Stark Law exceptions for non-physician practitioners
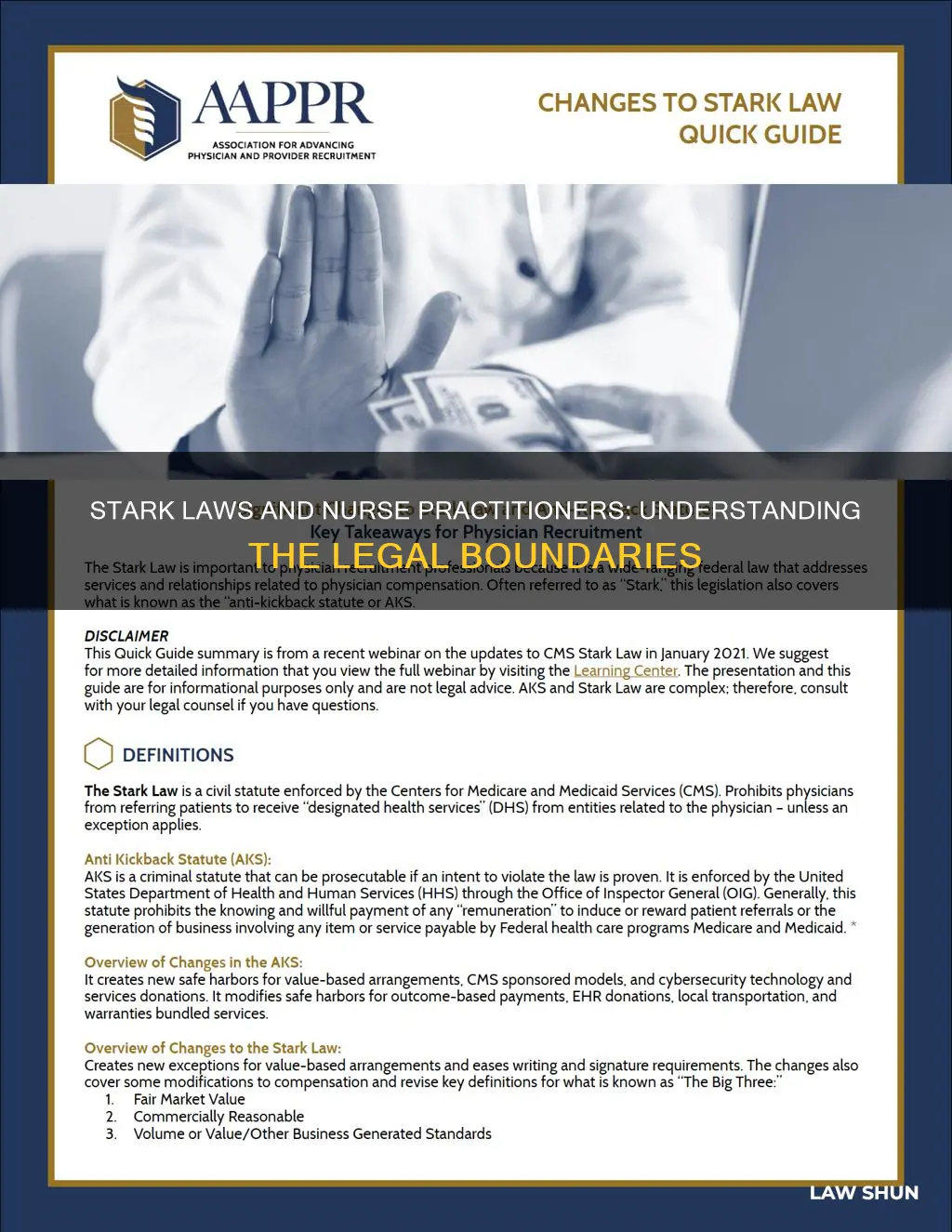
The Stark Law, or the Federal physician self-referral prohibition, is a set of regulations that limit the financial and business relationships that physicians may enter into. The law was enacted in 1992 and initially applied to physician referrals for clinical laboratory services. However, it has since been expanded to include "designated health services" (DHS), such as physical and occupational therapies, radiology services, medical equipment, inpatient hospital services, and more. The Stark Law is designed to prevent conflicts of interest and fraudulent testing, referrals, and medical services.
While the Stark Law applies primarily to physicians, there are exceptions for non-physician practitioners (NPPs). As of January 1, 2016, a new exception allows hospitals to provide subsidies to physician practices for the recruitment of NPPs. This exception was created in response to predicted shortages of primary care practitioners and an increased demand for NPPs due to healthcare initiatives and demographic changes. The Centers for Medicare and Medicaid Services (CMS) approved an NPP recruitment exception that includes subsidies for physician assistants, nurse practitioners, certified nurse midwives, clinical social workers, and psychologists.
It is important to note that the NPP exception comes with specific requirements and potential hazards. Hospitals must be cautious of potential abuses and inequities in NPP subsidy arrangements. Additionally, NPP subsidies do not implicate the Stark Law unless the NPP compensation arrangement serves as a "conduit" for prohibited physician referrals. CMS has warned about the potential for physicians to "game" the system, and hospitals should establish their own NPP subsidy limitations and guidelines to prevent abuses.
While the NPP exception provides hospitals with a tool for attracting new practitioners, it is crucial for hospitals to understand the intricacies of this exception to avoid potential legal and financial issues.
Child Labor Laws: US Territories' Compliance
You may want to see also

Nurse practitioners can perform tasks traditionally done by physicians
Nurse practitioners (NPs) are advanced practice registered nurses who have undergone additional training beyond that of a registered nurse. They are skilled in certain aspects of medical care traditionally performed by physicians. The role of the nurse practitioner emerged in the mid-1960s due to a growing need for primary care providers, particularly in rural and underserved areas.
Nurse practitioners can perform many tasks traditionally done by physicians, including:
- Diagnosing and treating acute and chronic conditions
- Ordering, conducting, and interpreting diagnostic tests
- Prescribing medications and other treatments
- Promoting health and disease prevention
- Conducting physical examinations
- Taking detailed health histories
- Drawing blood and other fluids
- Checking and documenting vital signs
- Educating patients about their care and treatment
- Providing moral support to patients
The scope of practice for NPs varies by state. Some states grant "full practice" status to NPs, allowing them to assess, diagnose, interpret diagnostic tests, and initiate treatment plans without supervision. Other states may require NPs to work under the supervision or collaboration of a physician, especially when prescribing medications.
While nurse practitioners have additional training beyond registered nurses, it is important to note that they have different educational requirements and training durations compared to physicians. Nurse practitioners typically need a Bachelor of Science in Nursing (BSN) and a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP). In contrast, physicians must complete four years of medical school to obtain an MD or DO degree, followed by three to seven years of residency and fellowship training.
Stark Law and Its Applicability to Medicaid Patients
You may want to see also

The Anti-Kickback Statute and its relation to nurse practitioners
The Anti-Kickback Statute (AKS) is a federal law that prohibits the solicitation or receipt of any form of remuneration in exchange for referrals to services covered by federal healthcare programs. The law aims to prevent overutilization and fraud by penalizing those who offer or accept kickbacks, bribes, or rebates for referrals or recommendations.
Nurse Practitioners (NPs) play an increasingly crucial role in healthcare delivery, and their services are in high demand across various hospital units. NPs can provide efficient and effective care, improve patient diagnosis and treatment, and support physicians in their daily rounds and responsibilities. However, the involvement of NPs in providing services that are traditionally the purview of attending physicians has raised questions about potential violations of the Anti-Kickback Statute.
In a recent advisory opinion, the Office of Inspector General (OIG) clarified the application of the Anti-Kickback Statute in the context of NPs performing services for referring physicians. The OIG concluded that while the arrangement constitutes remuneration, they would not impose administrative sanctions due to the minimal risk of fraud and abuse in the specific circumstances presented. This opinion is a departure from the OIG's usual stance of restricting arrangements involving remuneration between hospitals and referring physicians.
To ensure compliance with the Anti-Kickback Statute, hospitals must implement several safeguards. These include restricting the arrangement to specific units or specialties, maintaining daily communication between NPs and physicians, and stipulating that physicians cannot bill for the services performed by NPs. Additionally, hospitals should not provide remuneration to treating physicians for these arrangements, and they should not separately bill any payer for the NP services.
It is important to note that the OIG advisory opinion only applies to the specific scenario presented and may not cover all potential applications of NPs in healthcare delivery. Hospitals and healthcare providers should exercise caution and seek legal advice when structuring similar arrangements to ensure compliance with the Anti-Kickback Statute, Stark Law, and other relevant regulations.
Understanding ADA Laws: Private Property Exemptions and Compliance
You may want to see also

The impact of the Affordable Care Act on the demand for nurse practitioners
The Affordable Care Act (ACA) has had a significant impact on the demand for nurse practitioners.
Firstly, the ACA has helped millions of people gain access to health insurance, which has, in turn, increased the demand for healthcare services, including those provided by nurse practitioners. This has amplified the existing nursing shortage, with nurses being required to care for a larger number of patients and spend more time with each patient. As a result, nurse practitioners, who have the expertise to clinically diagnose and prescribe treatments, have become increasingly important in providing care. They often conduct in-office or telehealth visits, especially for new ACA enrollees who may have chronic, untreated conditions and limited understanding of medical processes.
Secondly, the ACA has led to a rise in emergency room and urgent care facility visits, as more people seek help with their now easily accessible insurance. This has increased the workload for nurses and other healthcare professionals in these settings.
Thirdly, the ACA has directed recipients to outpatient treatment centres in their communities, creating more nursing jobs in these areas. This helps enhance diversity in the healthcare experience and frees up space in hospitals for patients with urgent or acute needs.
Finally, the ACA has created opportunities for nurse practitioners to serve a growing and newly insured patient population, particularly in communities with a shortage of family medicine physicians. Many registered nurses are pursuing nurse practitioner degrees to take advantage of this trend, and patients often prefer seeing nurse practitioners due to their focus on whole-person care.
Overall, the ACA has increased the demand for nurse practitioners by making healthcare more accessible and highlighting the important role they play in providing quality care to a larger portion of society.
Idling Laws: Do They Apply to Semi Trucks?
You may want to see also
Frequently asked questions
The Stark Law is the Federal physician self-referral law. It prevents conflicts of interest by stopping physicians from referring patients to a service in which they have a financial interest.
Yes, nurse practitioners are covered by the Stark Law. They are defined as non-physician practitioners (NPPs).
Violating the Stark Law can result in fines, imprisonment, or both. Fines can be up to $15,000 per service and triple the amount of the improper payment.
One example is when a hospital provides payments or incentives to physicians to hire nurse practitioners without a proper arrangement in place. Another example is when a physician bills for services performed by a nurse practitioner.