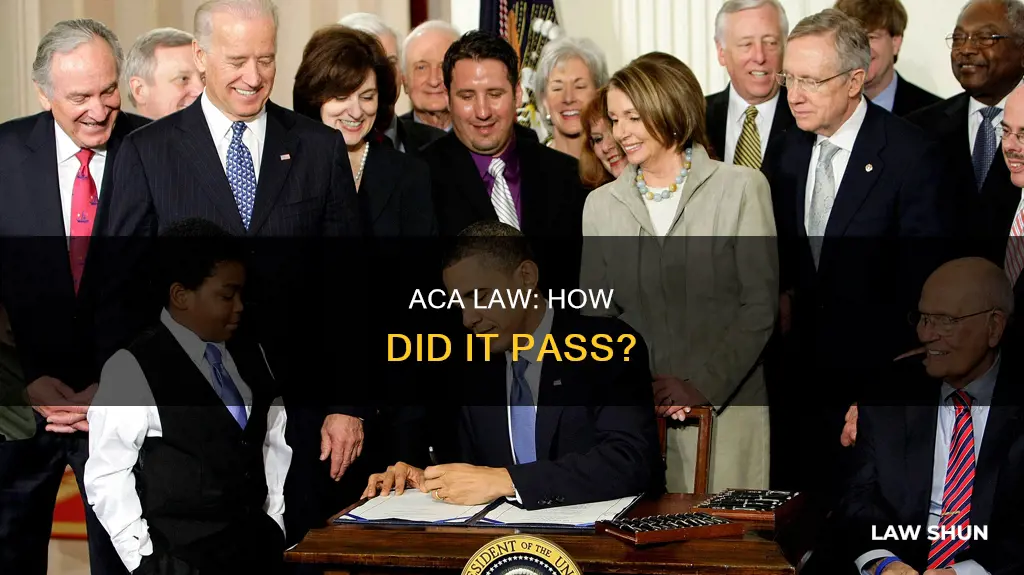
The Affordable Care Act (ACA), also known as Obamacare, was signed into law by President Barack Obama on March 23, 2010. The ACA is a landmark US federal statute that was enacted by the 111th United States Congress. The law was enacted in two parts: the Patient Protection and Affordable Care Act was signed into law on March 23, 2010, and the ACA was amended by the Health Care and Education Reconciliation Act on March 30, 2010. The ACA's major provisions came into force in 2014, and by 2016, the uninsured share of the population had roughly halved, with an estimated additional 20-24 million people covered.
| Characteristics | Values |
|---|---|
| Name | Affordable Care Act (ACA) |
| Other Names | Patient Protection and Affordable Care Act (PPACA), Obamacare |
| Type of Law | Landmark U.S. federal statute |
| Enacted By | 111th United States Congress |
| Signed Into Law By | President Barack Obama |
| Date Signed Into Law | March 23, 2010 |
| Amendments | Health Care and Education Reconciliation Act of 2010 |
| Goals | Make affordable health insurance available to more people, expand Medicaid to cover more people, support innovative medical care delivery methods to lower healthcare costs |
| Implementation Date | January 1, 2014 |
| Number of Titles | 10 |
What You'll Learn

The ACA's legislative goals
The Affordable Care Act (ACA) was signed into law by President Barack Obama in March 2010. The ACA's legislative goals are as follows:
Making affordable health insurance available to more people
The ACA provides consumers with subsidies (the "premium tax credit") that lower costs for households with incomes between 100% and 400% of the federal poverty level. If a household's income is above 400% of the federal poverty level, they may still qualify for the premium tax credit.
Expanding the Medicaid program to cover all adults with income below 138% of the federal poverty level
Not all states have expanded their Medicaid programs. However, the ACA's goal is to expand Medicaid to cover all adults with income below 138% of the federal poverty level.
Supporting innovative medical care delivery methods designed to lower the costs of health care
The ACA aims to support innovative medical care delivery methods to lower the overall costs of health care. This includes improving health care quality, efficiency, and accountability, as well as making strategic investments in the public's health.
Bill to Law: The Massachusetts Process
You may want to see also

The ACA's enactment
The Affordable Care Act (ACA), also known as Obamacare, was signed into law by President Barack Obama on March 23, 2010. The ACA was enacted to address health insurance coverage, health care costs, and preventive care. The law was enacted in two parts: the Patient Protection and Affordable Care Act, and the Health Care and Education Reconciliation Act, which was passed on March 30, 2010.
The ACA was a landmark piece of legislation, representing the most significant regulatory overhaul and expansion of coverage in the U.S. healthcare system since the enactment of Medicare and Medicaid in 1965. The law's major provisions came into force in 2014, and by 2016, the uninsured share of the population had roughly halved, with an estimated additional 20 to 24 million people covered.
The ACA had three primary goals:
- To make affordable health insurance available to more people, the law provided consumers with subsidies ("premium tax credits") that lowered costs for households with incomes between 100% and 400% of the federal poverty level.
- To expand the Medicaid program to cover all adults with income below 138% of the federal poverty level. However, not all states have expanded their Medicaid programs.
- To support innovative medical care delivery methods designed to lower the costs of health care generally.
In addition to establishing universal coverage and shared responsibility, the ACA set federal standards for health insurers, banning discriminatory practices based on age, gender, or health status. It also created state health insurance exchanges, simplified the enrollment process, and provided tax credits to make insurance more affordable for individuals and small businesses.
The enactment of the ACA faced strong political opposition, and there were calls for repeal and legal challenges. Despite this, the law had majority support by 2017, and it continues to shape the U.S. healthcare system today.
The Journey of a Bill to Becoming a Law
You may want to see also

The ACA's amendments
The ACA, or Affordable Care Act, was amended by the Health Care and Education Reconciliation Act on March 30, 2010. The ACA is a comprehensive health care reform law that was enacted in March 2010. The law has three primary goals:
- Make affordable health insurance available to more people.
- Expand the Medicaid program to cover all adults with income below 138% of the federal poverty level (FPL).
- Support innovative medical care delivery methods designed to lower the costs of health care generally.
The ACA's major provisions came into force in 2014. By 2016, the uninsured share of the population had roughly halved, with estimates ranging from 20 to 24 million additional people covered. The ACA amended the Public Health Service Act of 1944 and inserted new provisions on affordable care into Title 42 of the United States Code. The individual insurance market was radically overhauled, and many of the law's regulations applied specifically to this market.
The ACA has several major aims:
- Achieve near-universal coverage and do so through shared responsibility among government, individuals, and employers.
- Improve the fairness, quality, and affordability of health insurance coverage.
- Improve health-care value, quality, and efficiency while reducing wasteful spending and making the health-care system more accountable to a diverse patient population.
- Strengthen primary health-care access while bringing about longer-term changes in the availability of primary and preventive health care.
- Make strategic investments in the public's health, through both an expansion of clinical preventive care and community investments.
The ACA sets federal standards for health insurers offering products in both the individual and small-group markets, as well as employer-sponsored health benefit plans. These requirements considerably expand on federal standards first introduced as part of the Health Insurance Portability and Accountability Act of 1996. The ACA also encourages employers to undertake workplace wellness activities that promote and incentivize actual health outcomes.
Beyond subsidizing coverage and regulating the insurance and group health plan markets, the ACA creates state health insurance Exchanges for both individuals and businesses. Exchanges are meant to simplify and ease health insurance purchasing by creating a one-stop shopping market for insurance products that qualify for federal tax subsidies and that meet federal and state standards. Qualified health benefit plans sold inside or outside Exchanges will have to meet a series of federal requirements, including coverage of "essential benefits."
In addition to insurance reforms, the ACA begins the job of realigning the health-care system for long-term changes in health-care quality, the organization and design of health-care practice, and health information transparency. It does so by introducing broad changes into Medicare and Medicaid that empower both the Secretary of the U.S. Department of Health and Human Services (HHS) and state Medicaid programs to test new modes of payment and service delivery.
The ACA also makes direct public health investments, including new regulatory requirements related to coverage of clinical preventive services without cost sharing, and the development of a national prevention plan and the establishment of a Prevention and Public Health Trust Fund to finance community investments that will improve public health. The Act also targets specific subpopulations for new public health and health investments, particularly in the area of Indian health care.
LD 1104: Is It Now Law?
You may want to see also

The ACA's insurance coverage reforms
The Affordable Care Act (ACA) was signed into law in March 2010 by President Barack Obama. It is a comprehensive health care reform law that aims to make affordable health insurance accessible to nearly everyone. Here are some key details about the ACA's insurance coverage reforms:
- Elimination of Pre-existing Condition Exclusions: Insurers are prohibited from denying coverage or charging higher premiums based on pre-existing conditions. This ensures that individuals with medical conditions such as diabetes or cancer have access to affordable insurance.
- Essential Health Benefits: The ACA mandates that all individual and group health plans cover essential health benefits, including ambulatory patient services, emergency services, hospitalization, maternity and newborn care, mental health services, prescription drugs, rehabilitative services, and more. These benefits are standardised across all plans, ensuring that consumers receive a minimum level of coverage.
- Prohibition on Lifetime and Annual Limits: The ACA eliminates lifetime limits on coverage and restricts annual limits. This protects consumers, especially those with high healthcare needs, from reaching coverage limits or losing their coverage.
- Dependent Coverage Expansion: The ACA allows young adults to remain on their parents' health plans until they turn 26, regardless of their living situation, tax dependency, or student status. This provision has helped millions of young adults gain health insurance coverage.
- Health Insurance Marketplace: The ACA established health insurance marketplaces in every state, where individuals and families can shop for and purchase health insurance. These marketplaces offer plans categorised into Bronze, Silver, Gold, and Platinum tiers, with varying levels of out-of-pocket costs and premiums.
- Premium Tax Credits and Cost-Sharing Reductions: The ACA provides subsidies in the form of premium tax credits to individuals and families with incomes between 100% and 400% of the federal poverty level. Additionally, cost-sharing reductions are available to lower out-of-pocket expenses for those who qualify.
- Summary of Benefits and Coverage (SBC): All health plans are required to provide a standardised and easy-to-understand summary of their benefits, known as the SBC. The SBC includes information about covered benefits, cost-sharing requirements, and examples of how the plan would cover care for specific health conditions.
- Preventive Services Coverage: The ACA mandates that private health insurance plans cover a range of preventive health services without any patient cost-sharing. This includes routine immunisations, preventive services for children and youth, and preventive health services for women, such as well-woman visits and contraceptive coverage.
- Extension of Medicaid Eligibility: The ACA expanded Medicaid eligibility to all Americans with incomes below 138% of the federal poverty level. However, the Supreme Court ruled in 2012 that states have the option to opt out of this expansion, and not all states have chosen to expand their Medicaid programs.
- Medical Loss Ratio (MLR) Requirements: The ACA limits the amount of premium dollars insurers can spend on administration, marketing, and profits. Insurers are required to spend at least 80% of premiums on healthcare claims and quality improvement, with higher standards for large group markets. Insurers who do not meet these thresholds must issue rebates to consumers.
- Risk Adjustment, Reinsurance, and Risk Corridors: The ACA includes provisions to promote premium stability, particularly during the early years of implementation. These mechanisms encourage insurers to participate in the marketplaces and compete based on quality and value rather than avoiding high-risk enrollees.
- Health Plan Benefit Design: The ACA sets uniform standards for covered benefits and cost-sharing in the individual and small group markets. This ensures that consumers know what to expect in terms of coverage and out-of-pocket costs when purchasing insurance.
The Legislative Process: How a Bill Becomes Law
You may want to see also

The ACA's implications for public health policy and practice
The Affordable Care Act (ACA) has had a profound impact on public health policy and practice in the United States. Here are some key implications:
Expanded Access to Health Insurance
The ACA's primary goal was to increase access to affordable health insurance for more Americans. This was achieved through a combination of Medicaid expansion and the creation of health insurance exchanges, resulting in a near-universal guarantee of coverage. This expansion of coverage included support for innovative medical care delivery methods and a focus on preventive care.
Improved Health Insurance Coverage
The ACA introduced a range of reforms to improve the fairness, quality, and affordability of health insurance. It prohibited insurers from denying coverage or charging higher premiums based on pre-existing conditions and placed limits on annual and lifetime coverage caps. The law also mandated essential health benefits, such as ambulatory patient services, emergency services, hospitalization, maternity and newborn care, and mental health services.
Strengthened Primary Health Care
The ACA made significant investments in strengthening primary health care, particularly in medically underserved communities. It provided funding for community health centers and the National Health Service Corps, aiming to double the number of patients served. This expansion improved access to primary care services, especially for low-income and underserved populations.
Enhanced Preventive Care and Public Health Investments
The ACA placed a strong emphasis on preventive care, ensuring that clinical preventive services were covered without cost-sharing. It established a National Prevention, Health Promotion, and Public Health Council and created a Prevention and Public Health Trust Fund to finance community investments in public health. These measures represented a fundamental shift in the relationship between health insurance and preventive care.
Increased Data Availability for Public Health
The ACA imposed data obligations on health insurance exchanges and qualified health plans, requiring them to collect and report various data points. This has resulted in a wealth of information on enrollment, health care utilization, and performance metrics. Public health agencies can leverage this data to improve their understanding of population health and the effectiveness of health interventions.
Transformed Relationship Between Americans and the Healthcare System
The ACA reframed the financial relationship between Americans and the healthcare system. By introducing an individual mandate and shared responsibility among government, individuals, and employers, the law aimed to stabilize the insurance market and reduce the number of uninsured. This shift had far-reaching implications for how individuals interact with the healthcare system.
Challenges and Opportunities for Public Health Agencies
The ACA presented both challenges and opportunities for public health agencies. With the expansion of coverage, public health agencies had to navigate the complex landscape of collaborating with health insurance exchanges, Medicaid agencies, and health care providers to ensure optimal care for their communities. They also had to adapt to the changing nature and mission of public health within the context of universal health coverage.
The Lawmaking Process: From Bill to Law
You may want to see also
Frequently asked questions
The ACA, or Affordable Care Act, is a comprehensive health care reform law enacted in 2010. It has three primary goals: to make affordable health insurance available to more people, to expand the Medicaid program to cover all adults with income below 138% of the federal poverty level, and to support innovative medical care delivery methods designed to lower the costs of health care.
The ACA puts in place comprehensive health insurance reforms that rolled out over four years and beyond. Some of the key features include:
- A new Patient's Bill of Rights that protects consumers from the worst abuses of the insurance industry.
- Cost-free preventive services for many Americans.
- Accountable care organizations and other programs that help health care providers work together to deliver better care.
- Open enrollment in the Health Insurance Marketplace, where individuals and small businesses can compare health plans.
- Tax credits for middle- and low-income families to help cover the cost of insurance.
- An expansion of the Medicaid program to cover more low-income Americans.
The ACA was enacted by the 111th United States Congress and signed into law by President Barack Obama on March 23, 2010. It was amended by the Health Care and Education Reconciliation Act on March 30, 2010.