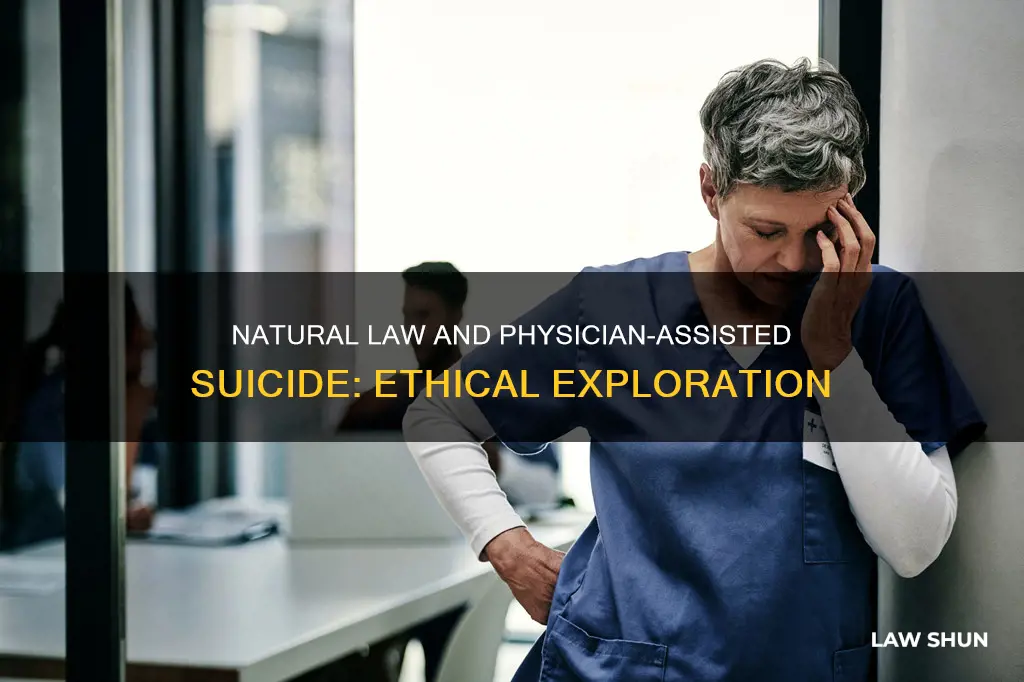
The topic of physician-assisted suicide is a highly controversial issue that has sparked intense moral debate. While some argue that it is a fundamental right for individuals to choose to end their lives with dignity, especially in cases of terminal illness or unbearable suffering, others believe that society has a moral duty to preserve all life. This conflict between individual autonomy and the sanctity of life presents a complex ethical dilemma. Proponents of physician-assisted suicide appeal to compassion and respect for individual choice, while opponents emphasise the potential risks and the importance of revering life. The legal status of physician-assisted suicide varies across different states and countries, reflecting the absence of a consistent standard that aligns with American conceptions of liberty, morality, and justice. This diversity in legal approaches underscores the need for a deeper exploration of the underlying principles and their implications.
| Characteristics | Values |
|---|---|
| Natural law and the "right to die" | Natural law can provide foundational principles for developing standards that are consistent with historical, philosophical, and political traditions |
| Physician-assisted suicide | Legal in some US states, prohibited at the federal level and in most states |
| Legal in some countries, including 10 US states, Canada, the Netherlands, and the Province of Victoria in Australia as of 2021 | |
| Misunderstood as being legal in Oregon due to the state's "Death with Dignity Act" | |
| Can be deemed homicide or euthanasia | |
| Can be seen as a violation of the integrity and ethics of the medical profession | |
| Can lead to voluntary or involuntary euthanasia | |
| Can be seen as a violation of the rights of doctors and nurses | |
| Can be seen as a violation of the right to life | |
| Can be seen as a violation of human dignity |
What You'll Learn

The right to die
The "right to die" is a highly contested topic that has sparked intense moral controversy. While some argue that individuals have the right to end their lives with dignity and free will, others believe that society has a moral duty to preserve life and prevent the devaluation of human life. This debate is particularly relevant in the context of physician-assisted suicide, where a medical professional aids a patient in ending their life.
Arguments for the Right to Die
Supporters of the right to die argue that individuals should have the freedom to choose what happens to their lives, including the right to end it when they deem necessary. This argument stems from the belief in individual autonomy and self-determination. Additionally, they contend that it is inhumane to allow individuals suffering from excruciating pain and terminal illnesses to continue enduring their condition. In such cases, providing assistance in ending their lives can be seen as an act of compassion and respect for their dignity.
Arguments Against the Right to Die
On the opposing side, those against the right to die argue that society has a fundamental duty to protect and preserve human life. Permitting assisted suicide, they believe, would violate this duty and devalue all lives. They worry that sanctioning such practices may lead to a slippery slope, where individuals with severe disabilities or the elderly may be pressured or urged to end their lives. Furthermore, they argue that assisted suicide would violate the rights and convictions of medical professionals who are opposed to the practice due to ethical reasons.
Natural Law and the Right to Die
Natural law theories, which have influenced the foundational principles of the United States Constitution, can provide a framework for understanding the "right to die" debate. By applying these theories, a consistent standard that aligns with historical, philosophical, and political traditions can be established to address these complex questions.
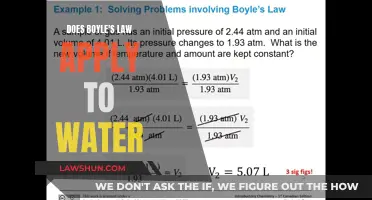
Physician-Assisted Suicide in Practice
As of early 2024, physician-assisted suicide has been legalized in several states, including Oregon, Washington, California, and Maine, through legislation or court rulings. However, it remains prohibited at the federal level and in most other states. The legalization of physician-assisted suicide highlights the distinction between what is legal and what is ethical. While a state may legalize the practice, it cannot force medical professionals who oppose it on ethical or personal belief grounds to participate.
Gay-Lussac's Law: Deflategate Explained
You may want to see also

The law and professional ethics
Physician-assisted suicide (PAS) is a highly contentious issue, with strong arguments for and against its legalisation. The topic raises questions about the role of the state, the rights of individuals, and the ethics of the medical profession.
The Law
In the US, the Supreme Court ruled in 1997 that state laws criminalising PAS were not unconstitutional, leaving it to individual states to decide whether to legalise or criminalise the practice. As of early 2024, 11 states and Washington, D.C. have legalised PAS, while 40 states have passed statutes prohibiting it, and 6 prohibit it by common law.
Professional Ethics
The American Medical Association's Code of Medical Ethics prohibits PAS in the same strong language it uses to prohibit physician involvement in euthanasia, stating that it is "fundamentally incompatible with the physician's role as healer".
However, some physicians argue that helping a patient who is determined to end their life can prevent greater harm, and that ending a patient's physical pain and mental anguish at their request does not violate the spirit or goals of medical ethics.
Those who support PAS legislation claim that all persons have a moral right to choose freely what they will do with their lives, as long as they inflict no harm on others. This right to free choice includes the right to end one's life. Supporters also argue that we have an obligation to relieve the suffering of our fellow human beings and to respect their dignity.
On the other hand, those who oppose PAS argue that society has a moral duty to protect and preserve all life, and that legalising PAS would violate the rights of doctors and nurses who may be pressured to cooperate in a patient's suicide, going against their own deeply held convictions.
Reconciling the Law and Professional Ethics
The legalisation of PAS in some states highlights the difference between what is legal and what is ethical. While a state may legalise PAS, it cannot force doctors who oppose the practice on ethical or personal belief grounds to participate. Physicians must navigate the complex landscape of legal and ethical considerations, weighing their obligations to their patients, their profession, and their own beliefs.
Housing Laws: Timeshare's Legal Loophole Explored
You may want to see also

The ethical issues of physician-assisted suicide
The Right to Die
The ethical debate surrounding physician-assisted suicide is complex and multifaceted. At its core, the issue revolves around the question of an individual's right to die, also known as euthanasia. Proponents of physician-assisted suicide argue that individuals should have the freedom to choose when and how they want to end their lives, especially in cases of terminal illness or unbearable pain. On the other hand, opponents argue that society has a moral duty to preserve and protect life, and that legalising assisted suicide could lead to a slippery slope where the lives of vulnerable individuals are devalued and put at risk.
Autonomy vs. Preservation of Life
One of the key ethical considerations in the debate is the tension between autonomy and the preservation of life. Proponents of physician-assisted suicide argue that individuals should have the right to self-determination and autonomy over their own bodies. This includes the decision to end their lives if they are suffering from a terminal illness or experiencing unbearable pain. On the other hand, opponents argue that society has a responsibility to protect human life and that legalising assisted suicide could lead to a disregard for the value of life.
Compassionate Relief vs. Sanctity of Life
Another ethical dimension to consider is the balance between providing compassionate relief from suffering and upholding the sanctity of life. Proponents of physician-assisted suicide argue that it is cruel and inhumane to deny the pleas of those who are suffering from excruciating pain and facing a dignified end to their lives. They believe that compassion demands that we respect the wishes of those who want to end their suffering. In contrast, opponents argue that while relieving suffering is important, it should not come at the cost of violating the fundamental principle of respecting human life.
Individual Rights vs. Societal Risks
The debate also raises questions about the balance between individual rights and societal risks. Proponents of physician-assisted suicide argue that individuals should have the right to make decisions about their own lives without imposing their beliefs on others. However, opponents argue that legalising assisted suicide could lead to coercion or pressure on vulnerable individuals to end their lives, especially those who feel like a burden on their families or society. There are concerns about the potential abuse or misuse of assisted suicide, and the risk of devaluing the lives of vulnerable groups such as the severely handicapped or the elderly.
Medical Ethics and Professional Duties
Physician-assisted suicide also raises ethical questions about the role and duties of medical professionals. While some doctors may support the idea of helping their patients end their suffering, others argue that it goes against the fundamental principles of medical ethics and the role of healers. The American Medical Association's Code of Medical Ethics, for example, prohibits physician-assisted suicide, stating that it is "fundamentally incompatible with the physician's role as a healer". Additionally, there are concerns about the potential impact on the integrity and ethics of the medical profession, as well as the risk of involuntary euthanasia.
In conclusion, the ethical issues surrounding physician-assisted suicide are complex and deeply divisive. While some argue for the right to die and the importance of autonomy and compassionate relief from suffering, others emphasise the sanctity of life and the potential risks to vulnerable individuals and society as a whole. The debate continues to be a subject of intense moral controversy, with individuals, societies, and medical professionals struggling to reconcile these conflicting ethical considerations.
Texas Abortion Law: Ectopic Pregnancy Exemption?
You may want to see also

The right to free choice
Proponents of physician-assisted suicide argue that this right to end one's life is one that most people can easily exercise. However, there are many who want to die but are unable to do so due to their disease, handicap, or condition. In such cases, they argue, individuals should be allowed to seek assistance in exercising their right to die, and their wishes should be respected.
Furthermore, supporters of physician-assisted suicide contend that we have an obligation to relieve the suffering of our fellow human beings and respect their dignity. They argue that it is cruel and inhumane to refuse the pleas of those suffering from excruciating and terminal conditions who beg for a merciful end to their pain and indignity. Compassion, they argue, demands that we comply and cooperate.
However, opponents of physician-assisted suicide argue that society has a moral duty to protect and preserve all life. They believe that allowing assisted suicide violates a fundamental duty to respect human life. They contend that a society committed to preserving life should not commission people to destroy it.
In conclusion, the right to free choice is a pivotal issue in the debate surrounding physician-assisted suicide. Supporters argue that individuals have the moral right to choose to end their lives and that this choice should be respected, especially when coupled with the desire to relieve suffering and preserve dignity. Opponents, however, maintain that society's duty to protect life supersedes the individual's right to choose, highlighting the tension between these two perspectives.
Wage Theft Protection Law: Do Government Workers Qualify?
You may want to see also

The risk of a slippery slope
The slippery slope argument against physician-assisted suicide (PAS) posits that legalising any form of euthanasia will inevitably lead to a gradual erosion of legal restrictions, ultimately resulting in non-voluntary or involuntary euthanasia. This argument has been present in the euthanasia debate since the 1930s, with critics warning that the acceptance of PAS will lead to the normalisation of concepts currently deemed unacceptable.
The logical version of the slippery slope argument claims that the initial acceptance of PAS will logically lead to the acceptance of involuntary euthanasia, as there is "no relevant conceptual difference" between the two practices. This version is supported by the observation that once PAS laws are passed, eligibility for assisted suicide tends to expand over time, putting more patients at risk. For example, in the Netherlands, what began as euthanasia permitted only for the terminally ill who requested it, eventually expanded to include the chronically ill, those with psychological suffering, and incompetent patients, including children. This expansion of eligibility criteria can lead to a creeping threshold of acceptability, potentially resulting in suicide contagion and a decrease in the taboo against suicide, which is an important piece of suicide prevention.
The "arbitrary line" version of the slippery slope argument suggests that the acceptance of PAS will lead to a series of small steps, each not significantly different from the previous one, eventually leading to the unacceptable outcome of involuntary euthanasia. This version does not rely on a logical connection between PAS and involuntary euthanasia but instead argues that it is impossible to justify accepting one while denying the other.
The empirical or psychological argument claims that the acceptance of PAS will, over time, lead to a moral change in society, resulting in the acceptance of involuntary euthanasia. While this argument requires strong evidence to support it, some studies have suggested that the legalisation of PAS in certain jurisdictions has indeed led to an increase in cases of euthanasia, including non-voluntary euthanasia. For example, a 1999 study by Jochemsen and Keown found that euthanasia in the Netherlands was not well-controlled, with a significant percentage of cases practised illegally. Additionally, Herbert Hendin argued that the situation in the Netherlands demonstrated a slippery slope in practice, with doctors' attitudes changing over time, moving from tightly regulated voluntary euthanasia to the acceptance of euthanasia for people with psychological distress and from voluntary to non-voluntary and potentially involuntary euthanasia.
However, it is important to note that not all studies support the slippery slope argument. Some research has found no evidence of a slippery slope effect, concluding that the legalisation of PAS in certain jurisdictions did not result in an increase in cases of euthanasia or a heightened risk for vulnerable populations.
In conclusion, the risk of a slippery slope associated with the legalisation of PAS is a complex and highly debated topic. While some argue that it will inevitably lead to an erosion of moral boundaries and an increased risk to vulnerable individuals, others claim that it is a scare tactic that fails to recognise the importance of individual freedom and the potential benefits of PAS in alleviating suffering.
Indeterminate Sentencing Laws: Understanding Their Application
You may want to see also
Frequently asked questions
By early 2024, physician-assisted suicide was legalized in 11 US states: Oregon, Washington, Montana, Vermont, California, Colorado, the District of Columbia, Hawaii, New Jersey, Maine, and New Mexico. However, it is prohibited on the federal level and in most states.
Supporters of physician-assisted suicide argue that all persons have a moral right to choose freely what they will do with their lives, including ending their lives when they choose. They also argue that we have an obligation to relieve the suffering of our fellow human beings and to respect their dignity.
Opponents of physician-assisted suicide argue that society has a moral duty to protect and preserve all life, and that allowing physician-assisted suicide would violate the rights of doctors and nurses who might feel pressured to cooperate in a patient's suicide, going against their own deeply held convictions.