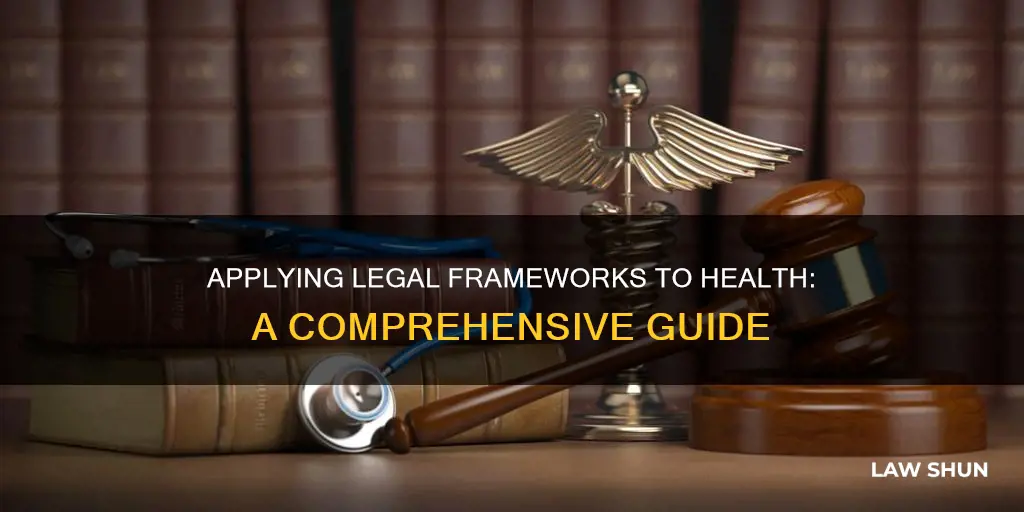
Health law is a diverse and complex field that governs the relationship between healthcare providers and patients. It involves interpreting legislation, representing clients, and navigating ethical considerations. Health lawyers play a critical role in ensuring fair and accessible healthcare, influencing public health outcomes, and contributing to the efficient administration of healthcare services. This field continues to grow and evolve, adapting to changes in telemedicine, healthcare technology, and health insurance regulations. The application of health law ranges from ensuring patient rights to guiding pharmaceutical companies through the approval process for new drugs.
| Characteristics | Values |
|---|---|
| Purpose | Protect and promote public health |
| Scope | Interpreting legislation, representing clients, and analyzing public health policy and bioethics |
| Focus | Healthcare services, insurance, privacy, and fraud |
| Education | LL.M., MPH, DrPH, MPA, PhD, JD |
| Experience | Minimum 4-5 years of law practice with substantial involvement in health law |
| Examination | Written exam and on-the-job training |
| Certification | Board Certified in Health Law |
| Recertification | Every 5 years |
What You'll Learn

Interpreting new legislation for employers and providers
As new laws and regulations are introduced, employers and providers must stay informed and ensure compliance with the relevant standards and requirements. This involves understanding the specific obligations and restrictions outlined in the legislation and making any necessary adjustments to policies, procedures, and practices. Here are some key considerations for interpreting new legislation:
- Understanding the Legislative Landscape: Interpreting new legislation requires a comprehensive understanding of the existing legal framework. This includes knowledge of federal, state, and local laws and regulations relevant to the industry. For example, in the healthcare industry, employers and providers must be aware of laws such as HIPAA, COBRA, and the Affordable Care Act.
- Staying Informed about Industry-Specific Laws: Different industries have unique regulatory requirements. For instance, the healthcare industry must comply with laws like EMTALA, which mandates the provision of emergency medical services regardless of a patient's ability to pay. Understanding industry-specific laws is crucial for effective interpretation and implementation.
- Monitoring Legislative Changes: Keeping abreast of legislative changes is essential. New laws and amendments can significantly impact employers' and providers' obligations. Staying informed allows for proactive planning and ensures compliance with the latest requirements.
- Seeking Expert Guidance: Interpreting complex legislation can be challenging. Seeking guidance from legal professionals or industry experts can help clarify obligations and ensure accurate interpretation. This is particularly important when dealing with rapidly evolving areas of law, such as health law.
- Implementing Necessary Adjustments: Once new legislation is understood, employers and providers must make any necessary adjustments to their policies, procedures, and practices. This may involve updating employee handbooks, changing operational protocols, or implementing new training programs to ensure compliance with the law.
- Ensuring Effective Communication: Clear and transparent communication about legislative changes is crucial. Employers should keep their employees informed about any new laws or regulations that may impact their work and provide training or guidance to ensure a smooth transition to the new requirements.
By following these considerations, employers and providers can effectively interpret and implement new legislation, ensuring compliance with the law and maintaining a harmonious and productive work environment.
Lease Laws: Cats in Charlotte, NC: What's the Verdict?
You may want to see also

Representing clients denied Social Security benefits
Understanding the Denial Reasons:
Start by carefully reviewing the Social Security Administration's (SSA) initial denial letter with your client. This letter will outline the specific reasons why their application for Social Security Disability Insurance (SSDI) or Supplemental Security Income (SSI) was denied. Common reasons for denial include earning too much income, a short-term disability, insufficient medical evidence, lack of communication with the SSA, or non-compliance with treatment. Understanding the exact denial reasons is crucial for developing an effective appeal strategy.
Gathering Evidence and Documentation:
Work with your client to gather comprehensive medical evidence and documentation to support their claim. This may include detailed medical records, doctor's evaluations, residual functional capacity forms, and official descriptions of their medical condition. If your client's condition has worsened or changed, be sure to submit this new medical evidence as it can significantly impact the appeal decision. Additionally, ensure that your client is compliant with any requested examinations or information by the SSA.
Meeting Income Guidelines:
Review your client's income to ensure it meets the SSA's definition of "substantial gainful activity." As of 2023, the monthly income limit for non-blind individuals is $1,470, while it is $2,590 for blind individuals. If your client's earnings exceed these thresholds, their application may be denied.
Appealing the Decision:
Guide your client through the appeals process, which typically involves multiple levels. The first step is usually to request reconsideration within 60 days of receiving the initial denial. During this stage, new evidence can be submitted, and your client has the right to representation by an attorney or disability advocate. If the reconsideration is denied, the next step is to request a hearing before an Administrative Law Judge (ALJ). This hearing provides an opportunity to present your client's case directly to the judge, who will then make a decision. If the ALJ's decision is unfavourable, the final level of appeal within the agency is to request a review by the Appeals Council.
Seeking Legal Representation:
Encourage your client to seek legal representation, especially during the appeals process. A qualified Social Security disability attorney can provide valuable guidance, ensure the protection of your client's rights, and improve their chances of a successful appeal. Disability attorneys typically work on a contingent fee basis, meaning they only receive payment if the client's case is successful.
It is important to stay organised, meet deadlines, and carefully follow the procedures outlined by the SSA throughout the appeals process. Each step typically has a time limit, and missing a deadline may result in having to start the application process over.
International Law: Can It Prevent Domestic Human Rights Abuses?
You may want to see also

Analysing public health policy and bioethics
Understanding Public Health and Bioethics
Public health is a societal approach that aims to protect and promote the health of populations rather than individuals. It focuses on collective actions, such as maintaining a safe water supply, immunising school children, and conducting epidemiological research, to create conditions that enable people to lead healthier lives. Bioethics, on the other hand, is a discipline that helps health professionals identify and address moral dilemmas in their work. While bioethics initially emerged in the contexts of medical care and human research, its principles are also applicable to public health.
Step 1: Identify Public Health Goals
The first step is to clearly define the goals of a public health program. These goals should ultimately be expressed in terms of reducing morbidity or mortality rates in the target population. For example, an HIV screening program should aim for fewer incident cases of HIV rather than just increasing testing rates. It's important to distinguish between proximate goals, such as increasing health literacy, and ultimate goals, which focus on improving health outcomes.
Step 2: Evaluate Program Effectiveness
This step involves examining the assumptions underlying a proposed intervention and assessing whether data supports these assumptions. For instance, a cardiac risk reduction program assumes that individuals will change their behaviour after receiving health information. However, behaviour change is often challenging to achieve, and programs should be evaluated based on their impact on morbidity and mortality rates.
Step 3: Identify Potential Burdens
The third step is to identify the potential burdens or harms associated with a public health program. These burdens may include risks to privacy and confidentiality, liberty, and justice. For instance, disease surveillance and reporting may raise privacy concerns, especially when data is individually identifiable. Additionally, some programs may disproportionately burden certain groups, requiring careful consideration of distributive justice.
Step 4: Minimise Burdens and Explore Alternatives
Once potential burdens are identified, the next step is to minimise them. This may involve modifying the program or exploring alternative approaches that achieve similar outcomes with fewer burdens. For example, in contact tracing, individuals have the right to refuse to disclose their partners' names or choose to inform their partners themselves.
Step 5: Ensure Fair Implementation
Fair implementation is crucial to ensuring that public health benefits and burdens are distributed equitably across communities. This means avoiding arbitrary or discriminatory targeting of specific populations without strong epidemiological justification. Additionally, it's important to consider the social consequences of allocating resources unequally to certain communities.
Step 6: Balance Benefits and Burdens
The final step is to weigh the expected benefits of a public health program against its identified burdens. This requires a democratic process that considers the views of all stakeholders, especially those from minority or vulnerable groups. While dissent is inevitable, it should be carefully considered, and highly burdensome programs should be subject to public hearings and scrutiny.
Understanding Lemon Law: Application and Duration
You may want to see also

Understanding the role of informed consent
Informed consent is a core principle of medical ethics and a legal requirement for medical treatment. It is the patient's right to fully understand and agree to any medical procedure or treatment before it can proceed. This is a basic ethical concept in medicine, but in practice, it can be more complicated.
Informed consent is an ethical concept first, a legal concept second, and finally, a formal administrative process. In the United States, informed consent laws vary by state and by circumstance. Some cases require a signed document indicating consent, while others only require a verbal agreement. However, in all cases, healthcare providers must keep some record of the process.
There are four elements to informed consent:
- The healthcare provider must verify that the patient has the capacity to understand and make decisions about their healthcare. If not, they must appoint a surrogate to make decisions on their behalf.
- The healthcare provider must disclose enough information for the decision-maker to make an informed choice.
- The healthcare provider must judge that the decision-maker understands the information.
- The decision-maker must freely authorize the treatment plan, usually with their signature.
Informed consent is a shared responsibility between the patient and the healthcare provider. The provider is obliged to inform the patient in the best way they know-how, and the patient may seek additional information from credible sources to reinforce their understanding.
Informed consent is a critical aspect of the doctor-patient relationship and ensures patients' rights are protected. It allows patients to play an active role in making decisions that affect their health and ensures their autonomy and independence are respected.
Energy Conservation Law: Temperature's Role Explored
You may want to see also

Applying for health coverage
To apply, you can use HealthCare.gov to apply online, which is the fastest way. Alternatively, you can apply over the phone, with help from people trained and certified by the Marketplace, or with agents and brokers who are trained professionals certified to sell health plans in their state. You can also apply through an approved enrollment partner, such as an insurance company or online health insurance seller. Finally, you can fill out and mail in a paper application to receive eligibility results within two weeks.
It is important to note that the deadline to enroll for health coverage starting January 1 is December 15.
Distracted Driving Laws: Eating While Driving in Minnesota
You may want to see also
Frequently asked questions
Health law is the body of law that regulates the provision of healthcare services and governs the relationship between healthcare providers and receivers. It covers a wide range of topics, from contracts and employment law to fraud and informed consent.
To become a health lawyer, you'll need to complete a law degree (a J.D.) and gain experience in the field. You can take introductory classes in health law to see if a particular aspect of the field interests you, and you may also want to consider an internship or fellowship to gain practical experience.
Some key health laws in the United States include the Social Security Amendments of 1965, the Emergency Medical Treatment and Active Labor Act (EMTALA), the Health Insurance Portability and Accountability Act (HIPAA), and the Patient Protection and Affordable Care Act.