Public health ethics involves a systematic process to clarify, prioritise and justify possible courses of public health action based on ethical principles, values and beliefs of stakeholders, and scientific and other information. The ethical principles that apply to public health laws include:
- Respect for autonomy
- Beneficence
- Non-maleficence
- Justice
- Solidarity or social cohesion
- Precautionary principle
These principles are applied to public health decision-making and action, which is often undertaken by governments and directed at the population level. The principles and values that guide public health ethics can differ from those that guide actions in biology and clinical medicine, which are more patient or individual-centred.
| Characteristics | Values |
|---|---|
| Non-maleficence | Do no harm |
| Beneficence | Produce benefit |
| Health maximisation | Maximise population health |
| Efficiency | Use scarce health resources efficiently |
| Respect for autonomy | Respect the autonomy of the patient |
| Justice | Equal opportunities and fair distribution of health outcomes |
| Proportionality | Weighing individual freedom against wider social goods |
What You'll Learn

Non-maleficence: Do no harm
The principle of non-maleficence, or 'do no harm', is a core principle in public health ethics. It is related to the Hippocratic 'primum nil nocere' or 'first, do no harm' of medical ethics. However, it is not identical, as it applies to public health policy and practice, which often involves 'trading off' degrees of harm to prevent greater harm or benefit the wider population.
The principle of non-maleficence asserts that public health professionals should act in a way that does no harm, even if their patients or clients request otherwise. This shifts the burden of proof onto those exercising potentially harmful behaviour to justify their actions.
For example, banning smoking in public places may harm individual smokers but will prevent greater harm (and benefit) the wider population by acting as a general disincentive to smoking.
Non-maleficence is one of the four commonly cited principles of biomedical ethics, along with beneficence, respect for autonomy, and justice. However, some scholars have identified up to seven mid-level principles, with non-maleficence being the first proposed due to its historical antecedence.
These seven principles are:
- Non-maleficence
- Beneficence
- Health maximisation
- Efficiency
- Respect for autonomy
- Justice
- Proportionality
Non-maleficence and beneficence can be understood in deontological and consequentialist terms. However, they do not seem to capture the core values of public health, as they tend to be associated with individual professional-client encounters rather than population health.
Therefore, the principle of health maximisation is proposed as a way to understand the ethical imperative to produce benefit in a wider sense, i.e., maximising health in the populations for which public health professionals are responsible.
The principle of non-maleficence is particularly relevant in situations where there is a tension between individual rights and broader conceptions of public benefit. In such cases, the burden of proof for restricting autonomy for wider public health goals should lie with those advocating restriction.
Applying to SMU Law Review: Tips and Tricks
You may want to see also

Beneficence: Act to produce benefit
The principle of beneficence, or 'do good', is one of the foundational principles of public health ethics. It is intimately connected to the principle of non-maleficence, or 'do no harm'. While non-maleficence is concerned with the omission of harmful action, beneficence is about taking active steps to benefit and help others.
In the context of public health, the principle of beneficence can be understood as an obligation to 'social beneficence' or to maximise health in the populations being served. This is a key distinction from medical ethics, where beneficence is often understood in the context of the individual doctor-patient relationship.
The obligation to produce benefit is a core principle within the Hippocratic tradition: physicians should heal and help their patients, according to their abilities and judgment. In public health, this translates to a duty to maximise health in the populations for which practitioners are responsible.
However, what constitutes 'benefit' is subject to dispute and may not be understood as simply 'health'. The concept of health itself is complex and contested, and the possibility of disagreement about what is being maximised is ever-present.
Despite this, the principle of beneficence remains a crucial guide for public health practitioners. It serves as a reminder that the primary end sought is the health and improvement of the broader constituency of the public, and that this should be measured by positive health outcomes.
The principle of beneficence is further nuanced by the idea of proportionality, which demands that individual freedom and wider social goods are weighed and balanced in a proportionate way. This means that any proposed intervention must be assessed in terms of its potential benefits and harms, and whether these are distributed fairly and justly.
Overall, the principle of beneficence is a vital component of public health ethics, guiding practitioners towards actions that produce benefit and improve the health of the populations they serve.
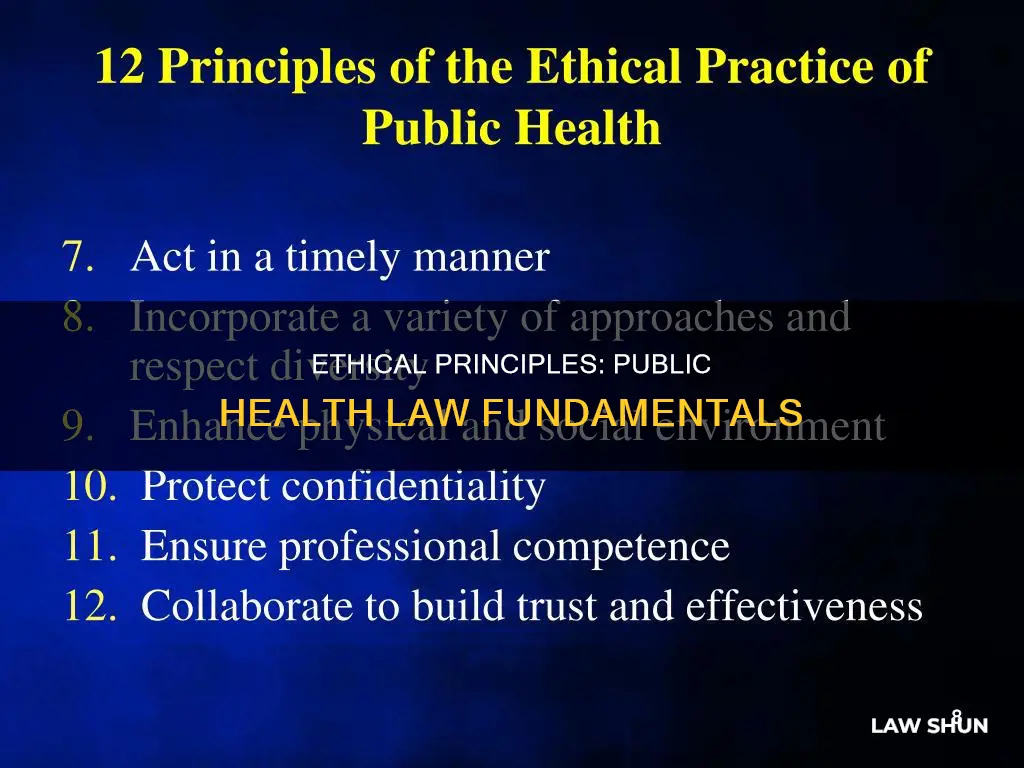
Examples and Applications
- Banning smoking in public places may cause harm to individual smokers but will prevent greater harms and benefit public health by acting as a general disincentive to smoking.
- Mandatory measles immunisation may infringe on parental and child autonomy but can be justified if it leads to better health outcomes for the wider population.
- Public health institutions should provide communities with information about policies and programs, especially when community consent is required for their implementation.
- Public health programs should incorporate diverse approaches that respect varying values, beliefs, and cultures in the community.
- Public health institutions should ensure the professional competence of their employees to act in the best interests of the public.
Understanding TWS Payday Law: Applicability to Contractors
You may want to see also

Health maximisation: Maximise population health
Health maximisation is a utilitarian approach to economic analysis that aims to produce the greatest population-wide number of a given outcome, such as the Quality-Adjusted Life Year (QALY), given certain budget constraints. However, this approach is problematic as it ignores distributional concerns and does not serve those in the poorest baseline health states.
To achieve health maximisation, healthcare resources would need to be allocated strictly in accordance with their marginal product, i.e., where they have the most benefit. This would mean that those in the poorest baseline health states would not be prioritised, as the yield (marginal product) of current treatments is usually low for this group.
Legislators and healthcare systems tend not to think in maximisation terms, instead focusing on protecting those with severe disabilities, cancer, and other life-threatening diseases. This is done through laws and policies that direct funds towards these groups and shield them from market forces.
To achieve health maximisation, a shift in focus is required towards prevention and population-wide measures. This could include policies such as seat belt regulation, unleaded gasoline, vaccination, and water fluoridation, as well as addressing the broader social and environmental determinants of health.
At an individual level, health maximisation can be achieved through a combination of clinical interventions and health-promoting behaviours such as exercise, diet, and social connections.
At a population level, health maximisation requires a coordinated set of strategies involving multiple sectors and partners working together to address the social, economic, and environmental determinants of health. This includes improving access to healthcare, addressing health disparities, and modifying social norms and values to support healthier behaviours.
Overall, while health maximisation has the potential to improve population health, it must be balanced with considerations of equity and social justice to ensure that the most vulnerable groups are not left behind.
Blue Laws in NJ: Electric Coffee Makers Included?
You may want to see also

Efficiency: Use scarce health resources efficiently
Efficiency is one of the six ethical principles that apply to public health laws. It involves using scarce health resources efficiently to maximise population health. This principle is based on the moral duty to use limited health resources efficiently to produce more health benefits for a larger number of people. It demands the use of evidence-based practices and cost-benefit analyses to determine the most effective and cost-efficient interventions. Efficiency in public health also involves sustainability and long-term effects, ensuring that interventions have a positive impact on the public's health over time.
The principle of efficiency in public health ethics recognises the scarcity of health resources and aims to maximise their impact. It is essential to consider both the immediate and long-term effects of public health interventions to ensure efficient use of resources. This includes evaluating the sustainability and cost-effectiveness of interventions to achieve the greatest health benefits for the population.
Public health professionals face the challenge of allocating limited resources effectively. They must consider the potential impact of their decisions on population health and strive to maximise benefits while minimising harm. This involves carefully evaluating the available evidence, considering the costs and benefits, and making informed decisions to optimise resource utilisation.
Additionally, the efficiency principle emphasises the importance of evidence-based practices and cost-benefit analyses in public health decision-making. By using scientific evidence and analysing the potential costs and benefits of different interventions, public health professionals can make more informed and efficient choices. This approach helps ensure that resources are allocated in a way that maximises health outcomes and minimises waste.
In conclusion, the efficiency principle in public health ethics emphasises the importance of using scarce health resources efficiently to maximise population health. It guides public health professionals to make informed decisions, considering both short-term and long-term impacts, to optimise resource allocation and improve health outcomes for the population.
Publicity Rights: Understanding the Law and Its Applications
You may want to see also

Respect for autonomy: Respect individual freedom and welfare
Respect for autonomy is a fundamental principle of public health ethics, recognising the importance of individual freedom and welfare within the community. This principle upholds the right of individuals to self-determination and respects their capacity for independent decision-making. While public health initiatives aim to improve community health, they must also consider the ethical implications for individual rights.
The principle of autonomy in public health acknowledges that individuals have the right to make choices regarding their health and well-being. This includes decisions about medical treatments, lifestyle choices, and participation in public health programmes. Respecting autonomy means recognising that individuals have the right to be informed, to consent or refuse treatment, and to make decisions based on their personal values and beliefs.
However, the complexity arises when individual autonomy conflicts with the collective good. Public health policies often involve preventative measures that benefit the community as a whole, and at times, these policies may infringe on personal autonomy. For instance, mandatory vaccination policies during the COVID-19 pandemic restricted individual freedom but were implemented to protect public health and safety.
To navigate these complexities, public health officials must carefully balance individual rights with the community's welfare. This involves considering the necessity, proportionality, and potential harm of public health interventions. Additionally, transparency, equity, and fairness in decision-making processes are crucial for respecting individual autonomy while also promoting the common good.
In conclusion, respecting individual autonomy in public health means upholding the right to self-determination, providing informed consent, and ensuring that policies are necessary, proportionate, and minimally restrictive. By doing so, public health officials can protect both individual freedom and the welfare of the community.
Maritime Law: Navigating Legal Waters
You may want to see also